Our Recipe for Healing
If you have recently looked up a recipe on the internet at any point in the last five years or so, you will notice that you have to scroll down through lengthy amounts of text of a back story, intermingled with photos of elements of the cooking process, ingredients, and the food itself until you are able to find the actual recipe. Prepare yourself for a similar experience here, as you learn how we are preparing to heal from what has taken place in the last week.
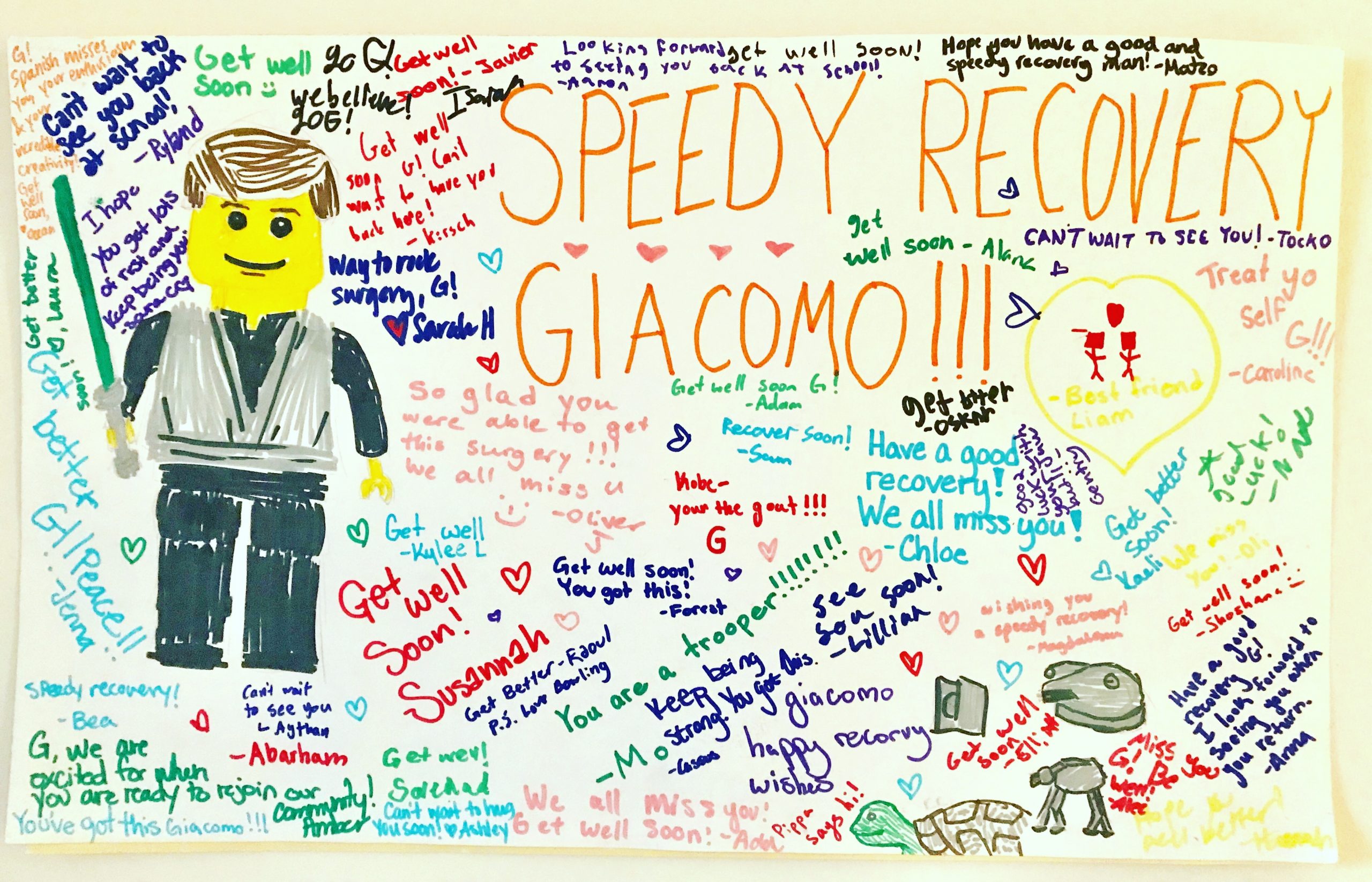
As you are likely aware, Giacomo’s surgery on Monday, May 20th to realign his jaw to improve swallowing, chewing, speech, and (now ironically) breathing was a grand success. Everything in the OR went as planned, with no real major hiccups in the operation itself. The postoperative experience has been many things, including but not limited to, traumatic, horrific, frustrating, and not what I hoped, yet fearfully anticipated, to say the least. (If you are unclear what I mean, go back to the blog and read the last few posts.)
However, here we are now, with G now needing to continue to be sedated and on a ventilator, with two partially collapsed lungs, one from the external respiratory efforts to save his life and one that is now collapsing due to the fact that he has been lying in bed, sedated on a ventilator for over five days now, due to the “unfortunate experiment” or “Tuesday’s event,” as it is being referred to here in the pediatric ICU. He will remain this way until next Thursday when he will have another surgery to have a tracheostomy tube placed. And yes, for those of you keeping track, this was the EXACT thing that had originally been planned as the safest, most effective way to breathe post-jaw surgery. What changed??
In digging deeper and talking to ALL of the providers who had a hand in Giacomo’s care, it would seem that his clinical pulmonologist gave a VERY false sense of security regarding his respiratory history and ability to the oral surgeons who prepared and performed his surgery, namely this whole idea that he would be able to breathe through a nasal mask on his BiPAP, once he was extubated. This BiPAP machine once provided me with  such an enormous amount of security at home, knowing that it was offering him ventilation overnight, allowing him to both inhale and exhale with necessary assistance, along with waking me up via alarms, should he decide to not breathe deeply enough or stop breathing altogether. Now, as it has sat at the head of his bed here in the PICU, the bed he nearly died in the other day, I am retraumatized every single time I look at it, remembering how they pulled out the only airway he had and attempted to make him use this machine to breathe in a way he never has. I hear those alarms, alarms that I once appreciated at home, as they woke me to run down the steep stairs from my bedroom to be at his side to rouse him enough start breathing again. Those alarms in my head are now a reminder of being by his side, as he stopped breathing completely, causing those alarms to sound perpetually, while my attempts to physically rouse him were completely futile, leaving me with my endless pleading to him to stay with me and not give up on life, while the medical team resuscitated him.
such an enormous amount of security at home, knowing that it was offering him ventilation overnight, allowing him to both inhale and exhale with necessary assistance, along with waking me up via alarms, should he decide to not breathe deeply enough or stop breathing altogether. Now, as it has sat at the head of his bed here in the PICU, the bed he nearly died in the other day, I am retraumatized every single time I look at it, remembering how they pulled out the only airway he had and attempted to make him use this machine to breathe in a way he never has. I hear those alarms, alarms that I once appreciated at home, as they woke me to run down the steep stairs from my bedroom to be at his side to rouse him enough start breathing again. Those alarms in my head are now a reminder of being by his side, as he stopped breathing completely, causing those alarms to sound perpetually, while my attempts to physically rouse him were completely futile, leaving me with my endless pleading to him to stay with me and not give up on life, while the medical team resuscitated him.
This false sense of security was transferred from the surgeons to the entire ICU staff, who believed G to be pretty much like other post-oral maxillofacial surgical patients, who could not only handle being extubated as soon as possible but would actually benefit greatly from that. Now, upon realizing that was NOT the case and that they should have listened to me, his mother, primary caregiver, and knower of all things G, the staff is listening. I have received many genuine apologies, along with behavior modification, which is all I require for forgiveness. We are moving forward together as a team. They have actually READ his chart, and they have had lengthy conversations with me and with each other to come up with this plan for placement of the trach tube. They have asked me questions about myotonic dystrophy. That super amazing ICU pulmonologist, the one who agreed with me on Monday night when I begged them not to pull him off the ventilator so soon has become Giacomo’s greatest advocate and resource. He actually seems to know the disease but is also wanting to learn more. He encou raged me to find other families with this disease who have had this same surgery to talk about their outcomes and care, so he can provide the best possible care for my guy. They are keeping him stable and working on building up his respiratory function and strength to prepare for next week’s surgery. They are getting to know his story, our family, and doing everything they possibly can to make our time here as good as it can be, which is important considering we will likely be here another 2 weeks after the trach tube is put in. And they are sending in things like these fancy boots were a gift from Physical Therapy to keep his feet in the proper alignment to prevent foot drop and reduce tension, (and yes, I am already planning to borrow them next winter since they are the coziest slippers I have ever seen!)
raged me to find other families with this disease who have had this same surgery to talk about their outcomes and care, so he can provide the best possible care for my guy. They are keeping him stable and working on building up his respiratory function and strength to prepare for next week’s surgery. They are getting to know his story, our family, and doing everything they possibly can to make our time here as good as it can be, which is important considering we will likely be here another 2 weeks after the trach tube is put in. And they are sending in things like these fancy boots were a gift from Physical Therapy to keep his feet in the proper alignment to prevent foot drop and reduce tension, (and yes, I am already planning to borrow them next winter since they are the coziest slippers I have ever seen!)
This ICU team is also staying on their toes, being forced (by me) to communicate fully and directly with me without fear of scaring me (I have explained that I have four kids with myotonic dystrophy and NOTHING scares me anymore,) and demonstrating that “waiting and seeing” is not a viable option. Just as I thought I was finishing this update of a good day, a solid plan, and stability, Giacomo decided to spike a fever that crept up to 103.2 in a matter of a couple of hours. I immediately feared infection, pneumonia, and also the possibility of him becoming septic. When the nurse , who was just coming on for her first shift with us tried to gently tell me that they needed to look into some things, I was the one who brought up all the possible things including the “S-Word,” as she called it, when I said, “I know you’re worried about this being sepsis.” From that moment on, she realized who she was working with, so she spent the next several hours getting labs checked, running cultures on urine, blood, and his lung secretions (which was not something they were originally planning to do, but I suggested.) We got chest x-rays, started more and different antibiotics and were able to help things move forward with my idea of giving G some electrolyte solution added to his G-Tube instead of more fluids or just plain water, as I know this guy is depleted. I had an incredibly restless night of attempted sleep, waking to every sound, including the end of a repositioning debacle that resulted in his oxygen saturation levels dropping down to 45%. This morning he is stable and we are all keeping a closer eye on things. In a lab somewhere in this hospital, they watching that bacteria from his lung secretions grow, secretions that thankfully his mother asked to have a culture from, so we can pinpoint exactly what antibiotic to treat this apparent infection.
, who was just coming on for her first shift with us tried to gently tell me that they needed to look into some things, I was the one who brought up all the possible things including the “S-Word,” as she called it, when I said, “I know you’re worried about this being sepsis.” From that moment on, she realized who she was working with, so she spent the next several hours getting labs checked, running cultures on urine, blood, and his lung secretions (which was not something they were originally planning to do, but I suggested.) We got chest x-rays, started more and different antibiotics and were able to help things move forward with my idea of giving G some electrolyte solution added to his G-Tube instead of more fluids or just plain water, as I know this guy is depleted. I had an incredibly restless night of attempted sleep, waking to every sound, including the end of a repositioning debacle that resulted in his oxygen saturation levels dropping down to 45%. This morning he is stable and we are all keeping a closer eye on things. In a lab somewhere in this hospital, they watching that bacteria from his lung secretions grow, secretions that thankfully his mother asked to have a culture from, so we can pinpoint exactly what antibiotic to treat this apparent infection.
So, while G is hanging out trying to heal, how are the other kids? How is Gigi? How am I?
As far as I can tell, the other kiddos are doing okay, though I miss them like crazy. Though I had originally thought it would not be good for them to see G on a ventilator, when I realized how long he would be this way, I did a risk-benefit analysis and decided they should come to see him. We’ve had a couple of visits so far, and they will spend a lot more time here next week after school, as things get  more stable and we work on weaning him off sedation. Seeing them and getting my fix of hugs was much-needed for all, plus Isadora was able to get me to spray a little more of my perfume on the scarves of mine she is wearing and sleeping with, as a comfort technique during this time away from me. If you are reading this and spend any amount of time with them, please give them lots of love and attention, but do be mindful that they are unaware of what happened with Giacomo on Tuesday, and believe his current state to be part of the healing from surgery, not know about his whole Code Blue event. Since at least one of them is likely to end up with this same surgery and they will all end up with multiple surgeries in their lifetimes, there really isn’t any need to contribute to more fear or anxiety, so please don’t mention it to them. (This picture is obviously not from today, but a Sunday morning about a month ago, and a prize I am keeping my eye on, in the hopes that all four of them will be bringing me coffee in the comfort of my own bed someday soon.) I also got word today that Barney, our cat, is feeling the stress too, so if you’re in our ‘hood, go give him a belly rub or cat treat or let him kill a mouse or two for you for his stress relief.
more stable and we work on weaning him off sedation. Seeing them and getting my fix of hugs was much-needed for all, plus Isadora was able to get me to spray a little more of my perfume on the scarves of mine she is wearing and sleeping with, as a comfort technique during this time away from me. If you are reading this and spend any amount of time with them, please give them lots of love and attention, but do be mindful that they are unaware of what happened with Giacomo on Tuesday, and believe his current state to be part of the healing from surgery, not know about his whole Code Blue event. Since at least one of them is likely to end up with this same surgery and they will all end up with multiple surgeries in their lifetimes, there really isn’t any need to contribute to more fear or anxiety, so please don’t mention it to them. (This picture is obviously not from today, but a Sunday morning about a month ago, and a prize I am keeping my eye on, in the hopes that all four of them will be bringing me coffee in the comfort of my own bed someday soon.) I also got word today that Barney, our cat, is feeling the stress too, so if you’re in our ‘hood, go give him a belly rub or cat treat or let him kill a mouse or two for you for his stress relief.
Gigi is managin g well, keeping herself occupied with the work of keeping our home and Enlightened Mama afloat and spending as much time here with us as possible, but just like the kiddos, please check in on her and give her some extra love and attention. We are two people who love this guy fiercely, going through the same experience, but in completely different ways. Support her and ask her how she’s doing. Make sure she gets food, coffee, chocolate, and bubbly water too (though I promise I am sharing with her, when she’s here with me at the hospital.) We are so grateful that her family surprised us and visited this weekend, giving her some much-needed laughter, distraction, intermingled with time hanging out in the ICU with us, in addition to the gift of Dr. Curious George, who now has the all-important role of supporting G’s intubation tube.
g well, keeping herself occupied with the work of keeping our home and Enlightened Mama afloat and spending as much time here with us as possible, but just like the kiddos, please check in on her and give her some extra love and attention. We are two people who love this guy fiercely, going through the same experience, but in completely different ways. Support her and ask her how she’s doing. Make sure she gets food, coffee, chocolate, and bubbly water too (though I promise I am sharing with her, when she’s here with me at the hospital.) We are so grateful that her family surprised us and visited this weekend, giving her some much-needed laughter, distraction, intermingled with time hanging out in the ICU with us, in addition to the gift of Dr. Curious George, who now has the all-important role of supporting G’s intubation tube.
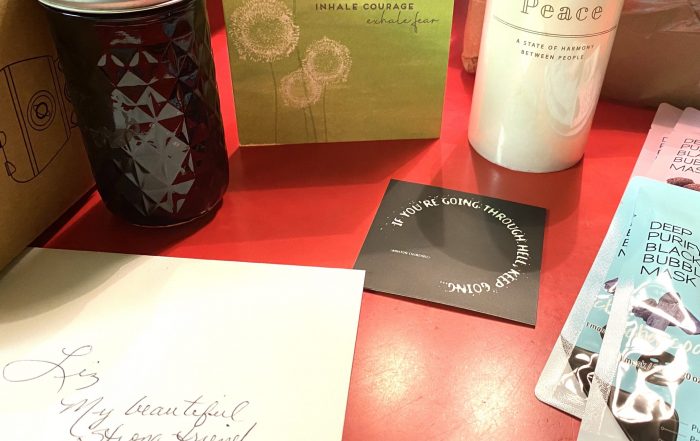
I am doing well, all things considered. Really. I rolled out my yoga mat in G’s room yesterday, where I found myself actually BREATHING for the first time all week. I am currently sitting on that same mat on the grass of the hospital lawn, enjoying the fresh air and sunshine for a few moments, while Gigi has taken over hand-holding for a bit. I am staying hydrated, maintaining my multi-beverage habit. I am asking people directly for what I need, something that is not easy but is so necessary right now. This has brought me many important things including, but not limited to, my mom and dental floss, along with all of the nourishment provided to us thus far, some of what has included surprises like this delicious nut mix, which was precisely what I neede d last night when too much craziness ensued and I was unable to eat dinner. (And yes, if you are bringing food, please bring more of this exact stuff, as I suspect more wild times and the need for quick bites may be ahead here over the next couple of weeks.) We are all surviving. We are far from out of the woods. We are so incredibly grateful for all of the love, support, food, prayers, donations, energy, visits, vibes, thoughts, chocolate, hugs, and everything else you all are sending our way. I am speechless when I see, read, feel, and experience what all of you are doing to hold us up during this rough time…and if you know me, being beyond words is a pretty darn rare occurrence. So again, thank you all for you have done and thank you in advance for what you will do in the future. We’ve got nothing but love and tons of hope, because of all of you.
d last night when too much craziness ensued and I was unable to eat dinner. (And yes, if you are bringing food, please bring more of this exact stuff, as I suspect more wild times and the need for quick bites may be ahead here over the next couple of weeks.) We are all surviving. We are far from out of the woods. We are so incredibly grateful for all of the love, support, food, prayers, donations, energy, visits, vibes, thoughts, chocolate, hugs, and everything else you all are sending our way. I am speechless when I see, read, feel, and experience what all of you are doing to hold us up during this rough time…and if you know me, being beyond words is a pretty darn rare occurrence. So again, thank you all for you have done and thank you in advance for what you will do in the future. We’ve got nothing but love and tons of hope, because of all of you.
And finally, the recipe for healing:
~8-10 days of sedation and ventilation
~2 types of antibiotics, but add more as needed
~1-2 daily doses of physical therapy
~1 team of doctors and nurses who work together, but also listen to the tiger mama in room C3128
~1 tracheostomy tube
~1 daily act of self-care, minimum
~1 removal of BiPAP machine from eyesight
~Food, beverages, and chocolate, as needed
Mix all this together with the continued love and support from our community, simmer for 2-3 weeks in the ICU, and you’ve got yourself some pretty amazing healing for G’Bot, and for this entire family.
“If you’re going through hell, keep going.”
For last night’s midterm, I needed to memorize the definition of the word “trajectory,” as it relates to one’s life, stated as “Relatively stable long-term processes and patterns of events, involving multiple transitions.” As I
The Coronavirus Slide
About five minutes before Gianna shot these pics of our spontaneous dancing to the Cha Cha Slide, (which I’m clearly not very skilled at, but do have the ability to laugh at myself whilst doing,)
Life Imitates Birth, As Per Usual
Nine months ago today, a new life was conceived. Nine months ago today, I began my day by walking my son into an operating room, for a pseudo-routine jaw surgery, as much as any surgery
Home is Where Your Nest Is
It's 1:49 in the morning. I am keeping watch over my son while he sleeps to ensure nothing happens to compromise his breathing and/or health. (These duties are shared by the nurse, who so kindly
Ooh Child…
Today, but a sheer stroke of luck, I had a break in my schedule. Instead of filling it with an appointment request, I took the time to go to a yoga class led by one
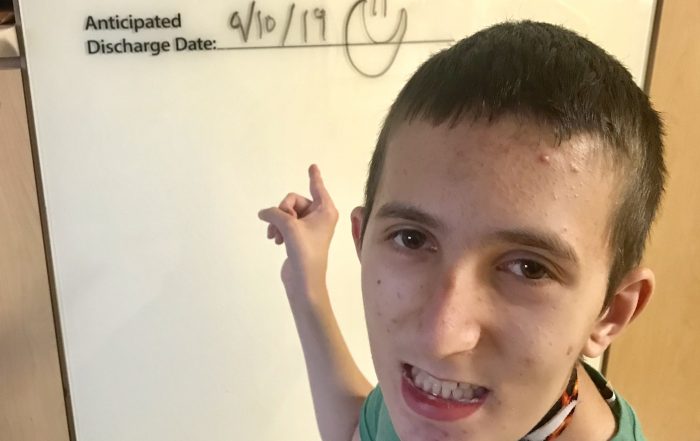
The Light at the End of the ICU Tunnel!
For over three months, I have looked at that white board in his room at the “Anticipated Discharge Date.” Blank. Empty. No ideas. (Save for Gianna who wrote a while back, “We don’t know.”) No end